Tibialis Posterior Tendinopathy?
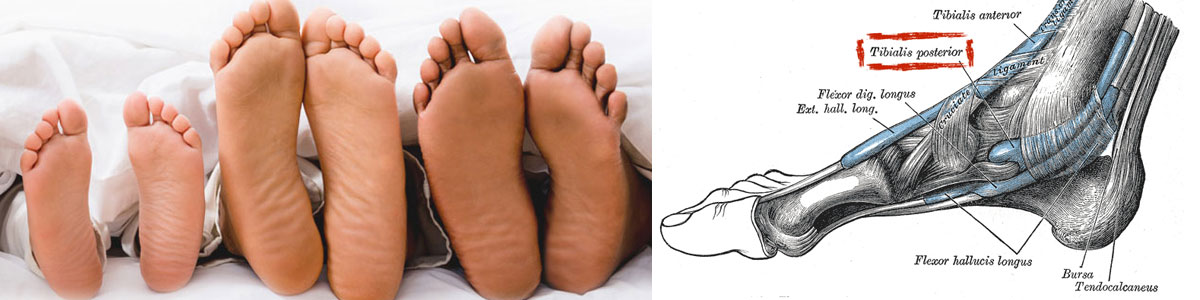
What is a Tibialis Posterior Tendinopathy?
The tibialis posterior muscle has a tendon that runs down the inside of your lower leg and behind your ankle bone (medial malleolus) and joins on to your midfoot. Its job is to help support our foot arch and to support your ankle.
The tendon can become painful at times causing you to be unable to run, jump or even walk without pain.
What are Tendons?
Tendons are the tough fibres that connect muscle to bone. Most tendon injuries occur near joints, such as the shoulder, elbow, knee, and ankle. A tendon injury may seem to happen suddenly, but usually, it is the result of many tiny tears to the tendon that have happened over time. Health professionals may use different terms to describe a tendon injury. You may hear:
Tendinitis (or Tendonitis): This actually means "inflammation of the tendon," but inflammation is rarely the cause of tendon pain.
Tendinosis: This refers to tiny tears in the tissue in and around the tendon caused by overuse.
Tendinopathy: This is an umbrella term that can refer to either tendinitis or tendinosis. As it is common to find areas of both tendinosis and tendinitis in the same tendon, the term tendinopathy is often used.
- Tibialis Posterior injuries can include:
- Tibialis Posterior tendinitis (an inflamed tendon).
- Tibialis Posterior tendinosis (a non-inflamed degenerative tendon).
- Tibialis Posterior tenosynovitis (an inflamed tendon sheath).
- a ruptured Tibialis Posterior tendon (secondary to degeneration or tear).
What Causes Tibialis Posterior Tendinopathy?
Tibialis Posterior Tendinitis or Tendinosis is nearly always caused by an overloading of the tendon especially where it curves around your ankle bone. The overloading of the tendon can be due to excessive weight, as in loaded calf raises, overtraining such as through a significant increase in running time or intensity, or a combination of the two such as an increase in jumping exercise or activities.
There are also certain biomechanical reasons why a Tibialis Posterior may not cope with an increase in load and these include poor foot posture, ankle joint stiffness, and even poor knee and hip control from weak or inhibited muscles. If the tendon has a degree of tendinosis, this weakens the tendon structure, which can lead to tendinitis if overloaded.
- Common Causes of Tibialis Posterior Tendinopathy include:
- Over-training or unaccustomed use – “too much too soonâ€Â
- A period of under-training, then moving back to previous training loads
- A sudden change in training surface – e.g. grass to bitumen
- Flat (over-pronated) feet
- Tight hamstring (back of thigh) and calf muscles
- Toe walking (or constantly wearing high heels)
- Poorly supportive footwear, or a change in footwear (even to new shoes!)
- Hill running
- Poor eccentric strength
How is Tibialis Posterior Tendinopathy Diagnosed?
Your physiotherapist or sports doctor can usually confirm the diagnosis of Tibialis Posterior tendinopathy in the clinic. They will base their diagnosis on your history, symptom behaviour and clinical tests.
Further investigations include US scan or MRI. X-rays are of little use in the diagnosis.
What are the Aims of Tibialis Posterior Tendinopathy Treatment?
Tibialis Posterior tendinopathy is a relatively common problem that we see at PhysioWorks and it is, unfortunately, an injury that often recurs if you return to sport too quickly – especially if a thorough rehabilitation program is not completed.
Researchers have concluded that there are essentially 7 stages that need to be covered to effectively rehabilitate these injuries and prevent recurrence.
What is the Treatment for Tibialis Posterior Tendinopathy?
Phase 1 - Early Injury Protection: Pain Reduction & Anti-inflammatory Phase
As with most soft tissue injuries the initial treatment is RICE - Rest, Ice, Compression and Elevation.
In the early phase you’ll be unable to walk without a limp, so your Tibialis Posterior tendon needs some active rest from weight-bearing loads. You may need to be non or partial-weight-bearing, utilise crutches, a wedged Achilles walking boot or heel wedges to temporarily relieve some of the pressure on the Tibialis Posterior tendon. Your physiotherapist will advise you on what they feel is best for you.
Ice is a simple and effective modality to reduce your pain and swelling. Please apply for 20-30 minutes each 2 to 4 hours during the initial phase or when you notice that your injury is warm or hot. Anti-inflammatory medication (if tolerated) and natural substances eg arnica may help reduce your pain and swelling. However, it is best to avoid anti-inflammatory drugs during the initial 48 to 72 hours when they may encourage additional bleeding. Most people can tolerate paracetamol as a pain reducing medication.
As you improve a rigid tape or kinesio-style supportive taping will help to both support the injured soft tissue.
Phase 2: Regain Full Range of Motion
If you protect your injured Tibialis Posterior tendon appropriately the torn tendon fibres will successfully reattach. Mature scar formation takes at least six weeks. During this time period, you should be aiming to optimally remold your scar tissue to prevent a poorly formed scar that will re-tear in the future.
It is important to lengthen and orientate your healing scar tissue via massage, muscle stretches, neurodynamic mobilisations, and eccentric exercises. Signs that you have full soft tissue extensibility includes being able to walk without a limp and able to perform Tibialis Posterior tendon stretches with a similar end of range stretch feeling.
Phase 3: Restore Eccentric Muscle Strength
Muscles work in two directions. They can shorten (called a concentric action) and lengthen in a controlled manner (called an eccentric action). Most Tibialis Posterior injuries occur during the controlled lengthening (eccentric) phase. Your physiotherapist will guide you on an eccentric Tibialis Posterior strengthening program when your injury healing allows.
Phase 4: Restore Concentric Muscle Strength
Calf strength and power should be gradually progressed from non-weight bear to partial and then full weight bear and resistance loaded exercises. You may also require strengthening for your other leg, gluteal and lower core muscles depending on your assessment findings. Your physiotherapist will guide you.
Phase 5: Normalise Foot Biomechanics
Tibialis Posterior tendon injuries can occur from poor foot biomechanics eg flat foot.
In order to prevent a recurrence, your foot will be assessed. In some instances, you may require a foot orthotic (shoe insert) or you may be a candidate for the Active Foot Posture Stabilisation program.
Your physiotherapist will happily discuss the pros and cons of both options to you.
Phase 6: Restore High Speed, Power, Proprioception & Agility
Most Tibialis Posterior tendon injuries occur during high-speed activities, which place enormous forces on your body (contractile and non-contractile). In order to prevent a recurrence as you return to sport, your physiotherapist will guide you with exercises to address these important components of rehabilitation to both prevent a recurrence and improve your sporting performance.
Depending on what your sport or lifestyle entails, a speed, agility, proprioception and power program will be customised to prepares you for light sport-specific training.
Phase 7: Return to Sport
Depending on the demands of your chosen sport, you will require specific sport-specific exercises and a progressed training regime to enable a safe and injury-free return to your chosen sport.
